A Short Textbook of PSYCHIATRY
Chapter 1. Diagnosis and Classification in Psychiatry
- Classification is a process organizing phenomena into categories based on resemblance and separation.
- Psychiatric disorders often lack distinct etiology, so syndromal classification based on clinical signs and symptoms is common.
- Three main purposes of psychiatric disorder classification: communication, comprehension of causes, and prediction of prognosis.
- A psychiatric disorder is defined as a disturbance in cognition, conation, or affect causing significant distress or disability, excluding socially deviant behaviors.
- Normal mental health is challenging to define but includes traits like reality orientation, self-awareness, self-esteem, voluntary behavior control, and productive activities.
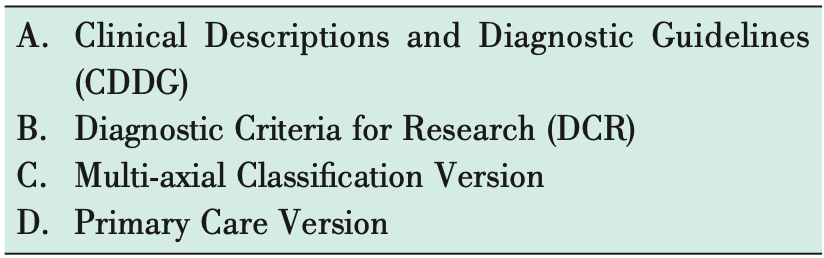
- Psychiatry’s classification systems, ICD-10 and DSM-IV-TR, have evolved to accommodate research findings on epidemiology, symptomatology, and treatment.
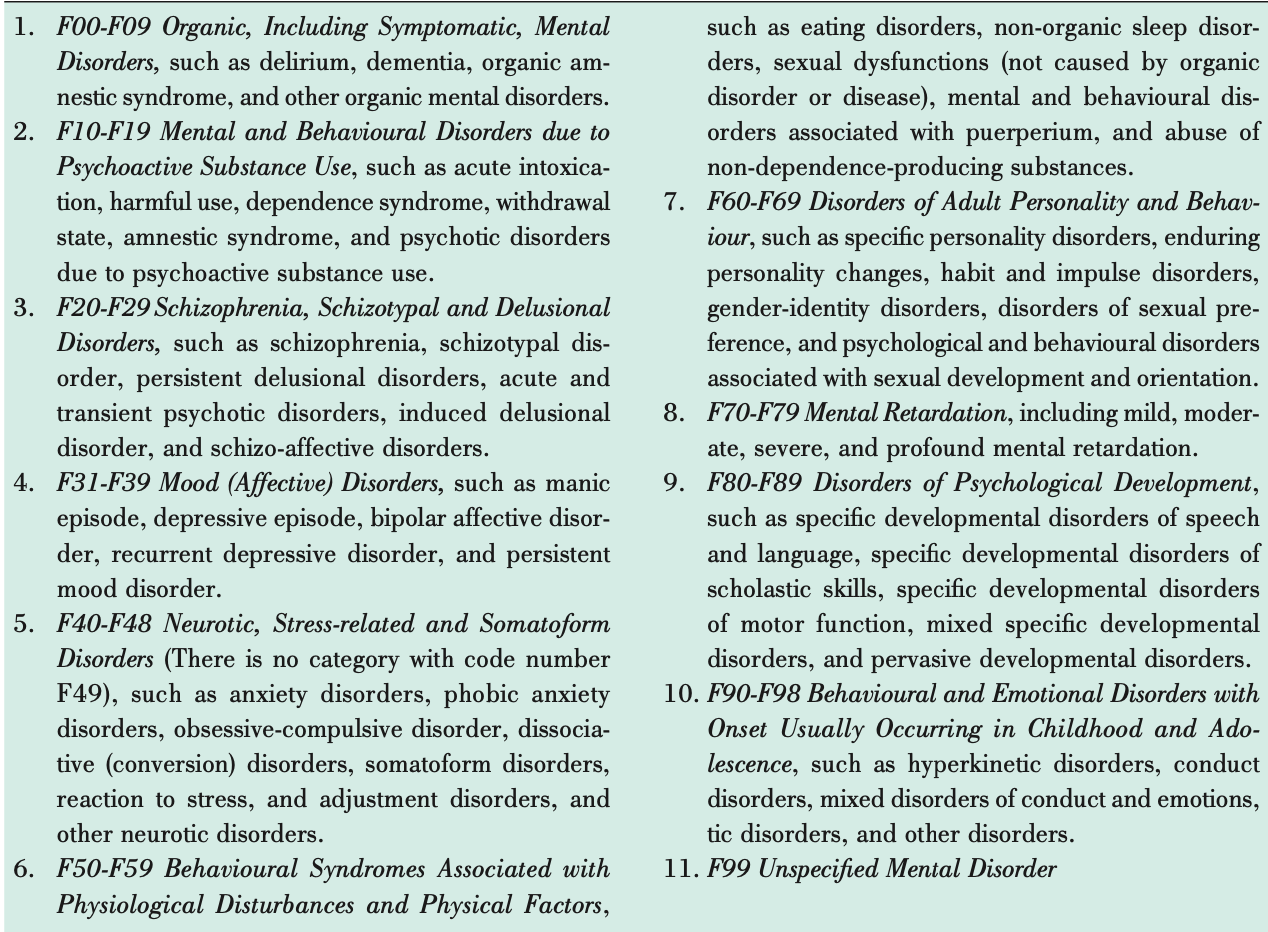
- ICD-10 classifies psychiatric disorders under Mental and Behavioral Disorders (MBDs) from F00 to F99.
- DSM-IV-TR is the American Psychiatric Association’s classification system.
- The next editions of ICD (ICD-11) and DSM (DSM-V) are expected in 2012-14.
- The book follows ICD-10 classification, although DSM-IV-TR criteria are discussed where appropriate.
- Earlier classifications relied on hierarchical diagnoses, but current systems allow for recording multiple diagnoses (co-morbidity).
- Considering co-morbidity helps identify and treat various aspects of a patient’s condition effectively.
- Making a correct diagnosis is crucial for evidence-based management but can lead to patient labeling and stigma.
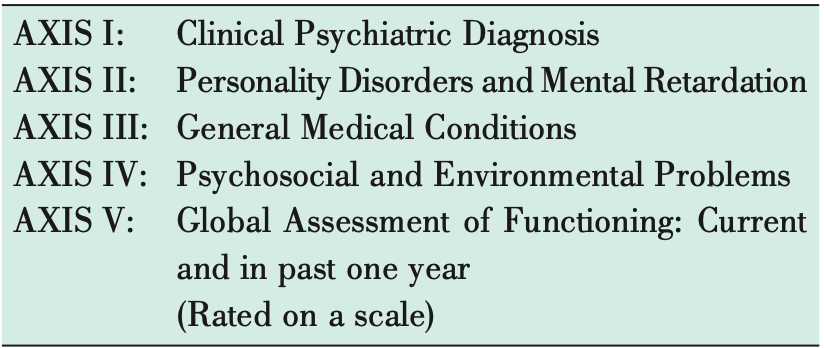
- Interest in multi-axial systems for comprehensive patient description has increased in recent decades.
- DSM-IV-TR utilizes a five-axis system for diagnosing individual patients, promoting thorough evaluation of needs.
- This approach allows for a holistic, biopsychosocial assessment of patients, considering various dimensions of their condition.
- ICD-10 has also introduced its own multi-axial classification version, enhancing the comprehensive evaluation of patients’ clinical problems and needs.
Chapter 2. Psychiatric History and Examination
- Familiarity with psychiatric assessment is crucial for medical practitioners and mental health professionals due to the prevalence of psychiatric symptoms in medical patients.
- The psychiatric interview holds significant importance in psychiatry, aiding in obtaining accurate information, establishing rapport, and improving adherence to treatment plans.
- A psychiatric interview differs from a routine medical interview in several aspects, emphasizing flexibility and empathic communication.
- Techniques such as observing verbal and non-verbal communication, using open-ended questions, and active listening are essential in psychiatric assessment.
- Confidentiality must be maintained, except in cases of risk to self or others.
- Comprehensive psychiatric assessment often requires multiple sessions and can be organized under various headings.
- Identification data, informants, and presenting complaints should be documented, with attention to detail and patient’s own words.
- History of present illness should include onset, duration, course, predisposing, precipitating, perpetuating, and relieving factors.
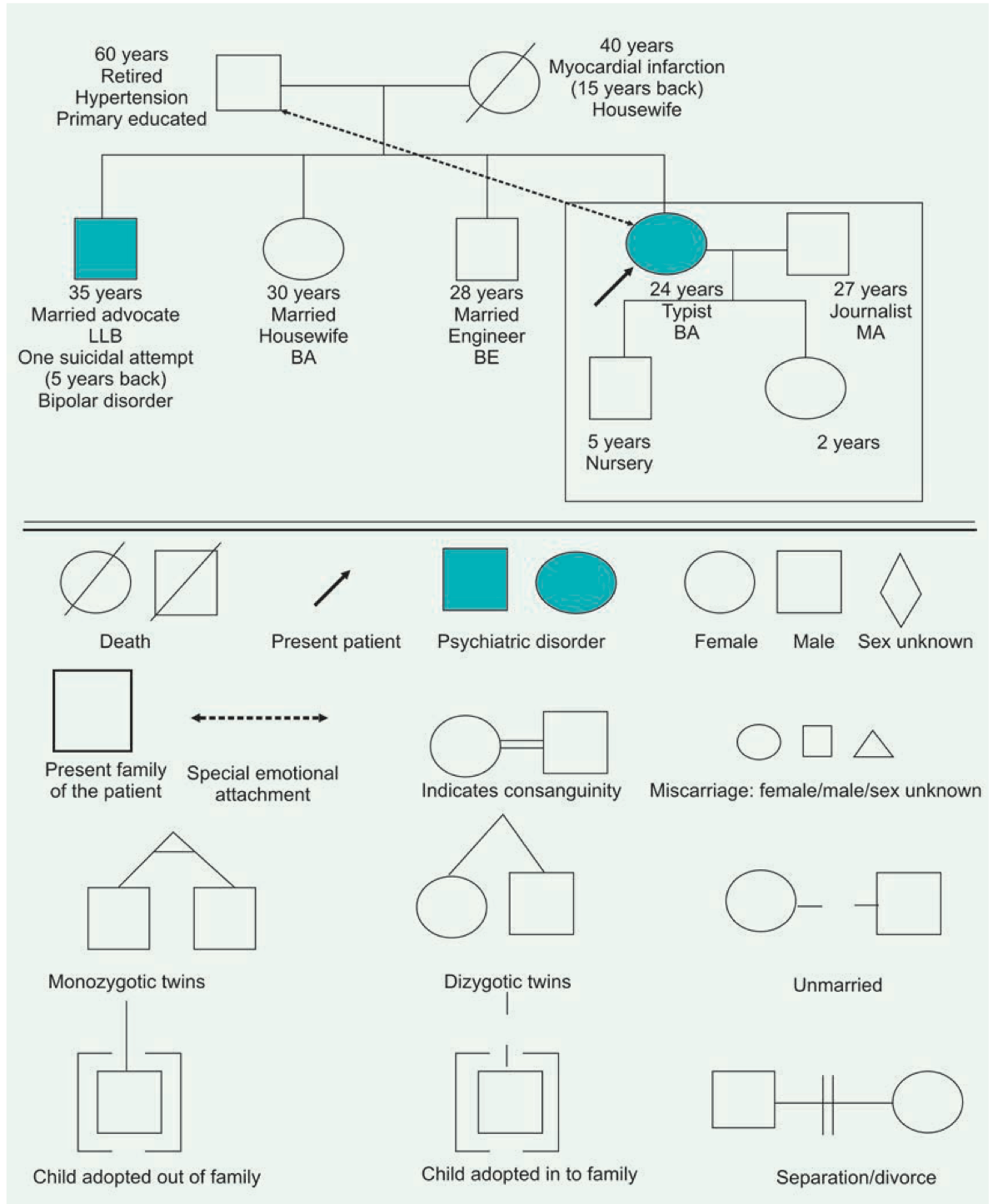
- Past psychiatric and medical history, treatment history, and family history are integral parts of psychiatric assessment.
- Family history should include family structure, history of psychiatric and medical illnesses, and current social situation.
- Communication patterns, affectivity range, cultural and religious values, and social support system should also be considered in family history assessment.
- Personal and social history is important in psychiatric assessment, especially for younger patients.
- Childhood history should include details of upbringing, developmental milestones, and any neurotic traits.
- Educational history encompasses academic achievements, relationships with peers and teachers, and any learning difficulties.
- Play history involves exploration of games played, peer relationships, and developmental stages.
- Puberty details include age at menarche, secondary sexual characteristics, and reactions to bodily changes.
- Menstrual and obstetric history covers menstrual regularity, pregnancies, and obstetric details.
- Occupational history includes job history, satisfaction, relationships at work, and appropriateness of job to educational background.
- Sexual and marital history involves sexual practices, relationships, marriages, divorces, sexual satisfaction, and contraceptive use.
- Premorbid personality assessment focuses on interpersonal relationships, leisure activities, mood, attitude towards self and others, work ethic, religious beliefs, fantasy life, and habits.
- Interviewing informants familiar with the patient prior to illness onset can provide valuable insight into premorbid personality.
- Alcohol and substance history is often recorded separately from personal history due to their significant impact on psychiatric symptoms and co-morbidity with psychiatric diagnoses.
- A detailed general physical examination (GPE) and systemic examination are essential to detect physical diseases that may contribute to psychiatric symptoms or be co-existent with psychiatric conditions.
- Mental status examination (MSE) is a standardized format to record psychiatric signs and symptoms during an interview.
- MSE covers areas such as general appearance and behavior, speech, mood and affect, thought, perception, cognition, insight, and judgment.
- General appearance and behavior assessment includes observation of cooperation, attentiveness, motor activity, posture, grooming, hygiene, and rapport with the examiner.
- Speech examination involves assessing rate, volume, flow, rhythm, and content of speech.
- Mood is described as the pervasive feeling tone, while affect is the outward expression of emotion.
- Thought examination includes assessment of stream and form of thought, as well as content, focusing on coherence, relevance, and presence of delusions or obsessions.
- Perception assessment includes hallucinations, illusions, depersonalization, derealization, and other sensory abnormalities.
- Cognition assessment evaluates consciousness, orientation, attention, concentration, memory, intelligence, and abstract thinking.
- Insight refers to the patient’s awareness and understanding of their illness, while judgment assesses their ability to assess situations and make appropriate decisions.
- Investigations, such as laboratory tests and psychological assessments, are conducted based on diagnostic and etiological possibilities identified during assessment.
- After assessment, a diagnostic formulation summarizes positive and negative information about the patient, lists differential diagnoses, prognostic factors, and outlines a management plan based on the biopsychosocial model.
- Special interviews may be necessary for specific populations, such as uncooperative, hostile, aggressive, or suicidal patients, as well as children.
Chapter 3. Organic (Including Symptomatic) Mental Disorders
- Psychological and behavioral processes, both normal and abnormal, are assumed to result from normal or deranged brain function.
- It’s a gross oversimplification to assume that all psychiatric disorders are organic solely because they involve abnormal brain functioning.
- According to current knowledge, psychiatric disorders can be broadly categorized into three types:
- Those with a known organic cause.
- Those where an organic factor hasn’t been identified.
- Those primarily due to psychosocial factors.
- Organic mental disorders are behavioral or psychological disorders associated with transient or permanent brain dysfunction. They include disorders resulting from demonstrable cerebral disease or disorder, either primary or secondary to systemic diseases.
- The term “organic” in this context doesn’t imply that other psychiatric disorders lack a biological basis. It simply means that organic mental disorders have a demonstrable and independently diagnosable cerebral disease or disorder.
- Given that organic brain illness can mimic psychiatric disorders, especially in early stages, organic mental disorder should be considered first in evaluating patients with psychological or behavioral clinical syndromes.
- Features requiring a high index of suspicion for organic mental disorder (organicity) include:
- First episode.
- Sudden onset.
- Older age of onset.
- History of drug and/or alcohol use disorder.
- Concurrent medical or neurological illness.
- Neurological symptoms or signs (e.g., seizures, impaired consciousness, head injury, sensory or motor disturbance).
- Presence of confusion, disorientation, memory impairment, or soft neurological signs.
- Prominent visual or other non-auditory hallucinations (e.g., olfactory, gustatory, tactile).
- These disorders can be subcategorized into:
- Delirium.
- Dementia.
- Organic amnestic syndrome.
- Other organic mental disorders.
Delirium
- Delirium is the most common organic mental disorder in clinical practice, affecting 5 to 15 percent of patients in medical and surgical inpatient units.
- It’s known by various names in the past, including acute confusional states, acute brain syndrome, acute organic reaction, toxic psychosis, and metabolic encephalopathies.
- Clinical features of delirium include:
- Relatively acute onset.
- Clouding of consciousness with decreased awareness of surroundings and ability to respond to stimuli.
- Disorientation, especially in time, followed by place and person.
- Perceptual disturbances such as illusions, misinterpretations, and hallucinations, often visual.
- Disturbance of sleep-wake cycle, with insomnia at night and daytime drowsiness.
- Impairment of new memory registration and retention.
- Psychomotor disturbance, typically agitation.
- Generalized autonomic dysfunction and speech and thought disturbances.
- Motor symptoms may include asterixis, multifocal myoclonus, carphologia or floccillation, occupational delirium, and tone and reflex abnormalities.
- Diagnosis of delirium can be missed, but early recognition is crucial as it may have a correctable underlying cause.
- Diagnosis is primarily clinical, and no specific laboratory test is diagnostic, although tests may help identify the underlying cause.
- According to ICD-10 criteria, delirium diagnosis requires symptoms in areas including impairment of consciousness and attention, global disturbance of cognition, psychomotor disturbances, sleep-wake cycle disturbance, and emotional disturbances.
- Delirium onset is usually rapid, with diurnal fluctuations and duration typically less than 6 months.
- Predisposing factors for delirium include various medical conditions, medications, and environmental factors.
- The etiology of delirium is diverse and can result from any factor sufficiently disrupting brain metabolism.
- Management involves identifying and correcting underlying causes, symptomatic measures such as benzodiazepines or antipsychotics for agitation, and supportive medical and nursing care.
- Investigations to determine the cause may include a battery of tests such as complete blood count, urinalysis, blood glucose, and imaging studies like CT scan or MRI.
Dementia
- Chronic organic mental disorder characterized by:
- Impairment of intellectual functions.
- Memory impairment, particularly recent memory.
- Deterioration of personality.
- Impairment occurs globally, affecting daily activities and relationships, with no impairment of consciousness (unlike delirium).
- Additional features may include emotional lability, catastrophic reaction, thought abnormalities, urinary and fecal incontinence, and disorientation.
- Diagnosis is clinical, with ancillary investigations aiding in determining underlying causes.
- ICD-10 criteria for diagnosis include evidence of decline in memory and thinking, impairment of daily activities, duration of at least 6 months, and clear consciousness.
- Differential diagnosis includes normal aging, delirium, and depressive pseudodementia.
- Types of dementia:
- Alzheimer’s Dementia: Commonest cause, characterized by progressive decline in memory and cognitive function. Diagnosis by exclusion, with treatment focusing on symptom management.
- Multi-infarct Dementia: Caused by multiple cerebral infarctions leading to progressive disruption of brain function. Characterized by abrupt onset, stepwise deterioration, and presence of hypertension or cardiovascular disease.
- Hypothyroid Dementia: Reversible cause of dementia due to hypothyroidism. Prompt treatment can lead to complete recovery if initiated within two years of onset.
- AIDS Dementia Complex: Cognitive, behavioral, and motor deficits in AIDS patients due to HIV’s neurotropic nature. Diagnosis via ELISA and Western Blot tests.
- Lewy Body Dementia: Second most common cause of degenerative dementias. Characterized by fluctuating cognitive impairment, visual hallucinations, and extrapyramidal symptoms.
- Management involves basic investigations to find underlying causes, environmental manipulation, treatment of medical complications, supportive care, and pharmacological interventions such as cholinesterase inhibitors or memantine for Alzheimer’s, antipsychotics for behavioral symptoms, and SSRIs for depression. Short-term hospitalization may be needed for emergent symptoms, while long-term placement may be necessary in later stages.
Organic Amnestic Syndrome:
- Characterized by:
- Impairment of memory due to an underlying organic cause.
- No severe disturbance of consciousness and attention (unlike delirium).
- No global disturbance of intellectual function, abstract thinking, and personality (unlike dementia).
- Memory impairment:
- Severe impairment of recent memory or short-term memory.
- Impaired remote memory or long-term memory.
- No impairment of immediate memory (immediate retention and recall).
- Confabulation may occur in the early phase, filling memory gaps, which often disappears as the disease progresses.
- Diagnosis according to ICD-10 requires recent memory impairment, no impairment of immediate retention and recall, attention, consciousness, global intellectual functioning, and historical or objective evidence of brain disease or injury.
- Differential diagnosis includes delirium, dementia, non-organic mental disorders, and transient global amnesia.
- Transient Global Amnesia: Resembles amnestic syndrome but with abrupt onset and patient distress due to memory loss.
- Aetiology:
- Thiamine deficiency (Wernicke-Korsakoff syndrome), often due to chronic alcohol dependence.
- Lesions involving bilaterally the inner core of limbic system.
- Management:
- Treatment of the underlying cause, such as thiamine for Wernicke-Korsakoff syndrome.
- Supportive care for general condition and treatment of associated medical illness.
Other Organic Mental Disorders:
- Associated with brain dysfunction due to primary cerebral disease, systemic disease (secondary), or toxic substances.
- Diagnosis based on evidence of cerebral disease, damage, or dysfunction, temporal relationship between disease development and mental syndrome onset, recovery from mental disorder following removal or improvement of underlying cause, and absence of evidence for an alternative cause.
- Risk Factors:
- Primary Cerebral Diseases: Epilepsy, limbic encephalitis, Huntington’s disease, head trauma, brain neoplasms, vascular cerebral disease, cerebral malformations.
- Systemic Diseases: Extracranial neoplasms, collagen diseases, endocrine disease, metabolic disorders, infectious diseases.
- Drugs: Steroids, propranolol, levodopa, antihypertensives, alcohol, hallucinogens.
- Organic Hallucinosis:
- Presence of persistent or recurrent hallucinations due to an underlying organic cause.
- Hallucinations can occur in any sensory modality, usually visual or auditory.
- Aetiology includes drugs, alcohol, sensory deprivation, sensory pathway diseases, epilepsy, intracranial lesions, and others.
- Management:
- Treatment of underlying cause if treatable.
- Symptomatic treatment with low-dose antipsychotic medication may be necessary.
Organic Catatonic Disorder:
- Diagnosis Criteria (ICD-10):
- Stupor (diminished or absent spontaneous movement with mutism, negativism, and rigid posturing).
- Excitement (hyperactivity with or without aggression).
- Mixed (rapidly shifting between hypo- and hyperactivity).
- Other catatonic symptoms and signs increase confidence in diagnosis.
- Aetiology: Detailed in Chapter 19.
- Management:
- Treat the underlying cause if possible.
- Symptomatic treatment with low-dose benzodiazepines or electroconvulsive therapy if necessary. Antipsychotics should be used cautiously.
Organic Delusional (Schizophrenia-Like) Disorder:
- Diagnosis Criteria (ICD-10):
- Presence of predominant delusions due to an underlying organic cause.
- Delusions vary depending on the etiology, often persecutory in nature.
- Hallucinations may accompany the delusions, usually visual rather than auditory.
- Diagnosis Difficulties: Distinguishing from paranoid schizophrenia, especially with amphetamine use.
- Aetiology:
- Drugs: Amphetamines, hallucinogens, cannabis, disulfiram
- Complex partial seizures (e.g. temporal lobe epilepsy)
- Huntington’s chorea (initial stages), Parkinson’s disease, Wilson’s disease, and idiopathic basal ganglia calcification
- Right parietal lobe lesions, especially vascular lesions
- Lesions involving limbic system (e.g. tumours) 6. Spinocerebellar degeneration
- Cerebral malaria
- Herpes simplex encephalitis
- Nutritional deficiencies (Vitamin B12, iron)
- Demyelinating disorders (such as multiple sclerosis, metachromatic leukodystrophy)
- Management:
- Treat the underlying cause, such as removing toxic agents in amphetamine psychosis.
- Symptomatic management with low-dose antipsychotic medication may be necessary.
Organic Mood (Affective) Disorder:
- Diagnosis Criteria (ICD-10):
- Prominent and persistent mood disturbance due to an underlying organic cause.
- Mood disturbance can be major depressive, manic, or mixed affective episode.
- Aetiology:
Drugs:
- Mania: Various drugs such as INH, Levodopa, Bromide, LSD, Corticosteroids (may cause hypomania), Hallucinogens, Tricyclic antidepressants, Cocaine, Baclofen, Amphetamines, Bromocriptine, Cimetidine, Procyclidine.
- Depression: Drugs like Reserpine, Ethanol, Clonidine, Methyldopa, Propranolol, Corticosteroids, Antipsychotics (especially typical antipsychotics), Cimetidine, Anticancer chemotherapy, Oral contraceptives. Any medication taken by a depressed individual should be considered a potential factor in causing depressive episodes.
Endocrine disorders:
- Mania: Hyperthyroidism.
- Depression: Conditions like Hypothyroidism, Cushing’s syndrome, Addison’s disease, hyper- and hypoparathyroidism can lead to depressive symptoms.
CNS disorders:
- Parkinsonism, Huntington’s chorea, PSP (progressive supranuclear palsy; more likely to cause depression), CVAs (cerebrovascular accidents; left-sided anterior lesions and right-sided posterior lesions may lead to depression), cerebral tumors, epilepsy (especially complex partial seizures), neurosyphilis (general paresis of the insane), head injury (more likely to induce mania), multiple sclerosis.
Post-viral illnesses:
- Conditions like Influenza, infectious mononucleosis, viral pneumonia, infectious hepatitis may trigger mood disorders.
Deficiencies:
- Pellagra, deficiency of thiamine, folate, niacin, and vitamin B12 can contribute to mood disorders.
Others:
- Carcinoma of the pancreas (associated with depression), Systemic Lupus Erythematosus (SLE), pernicious anemia, temporal arteritis (linked with depression), carcinoid syndrome (may lead to mania).
- Management:
- Manage the underlying organic cause if treatable.
- Symptomatic management depending on the episode severity, including mood stabilizers or antidepressants.
Organic Anxiety Disorder:
- Diagnosis Criteria (ICD-10):
- Prominent and persistent generalized anxiety or panic due to an underlying cause.
- Aetiology:
Drugs and toxins:
- Cocaine, caffeine, amphetamines, and other sympathomimetics, alcohol, and drug withdrawal, heavy metals, penicillin are associated with mood disorders.
Endocrine disorders:
- Dysfunction of thyroid, pituitary, parathyroid, or adrenal glands, pheochromocytoma, fasting hypoglycemia, carcinoid syndrome can contribute to mood disturbances.
Systemic diseases:
- Mood disorders can be influenced by cardiac arrhythmias, mitral valve prolapse syndrome, chronic obstructive pulmonary disease (COPD), coronary artery disease, pulmonary embolism, anemia, fever, and deficiency diseases.
CNS diseases:
- Mood disorders can result from cerebral tumors, epilepsy (especially complex partial seizures originating from the temporal lobe), cerebrovascular disease, and postconcussional syndrome.
- Management:
- Treat the underlying organic cause if possible.
- Symptomatic treatment with benzodiazepines, beta-blockers, or cognitive-behavioral therapy may be necessary.
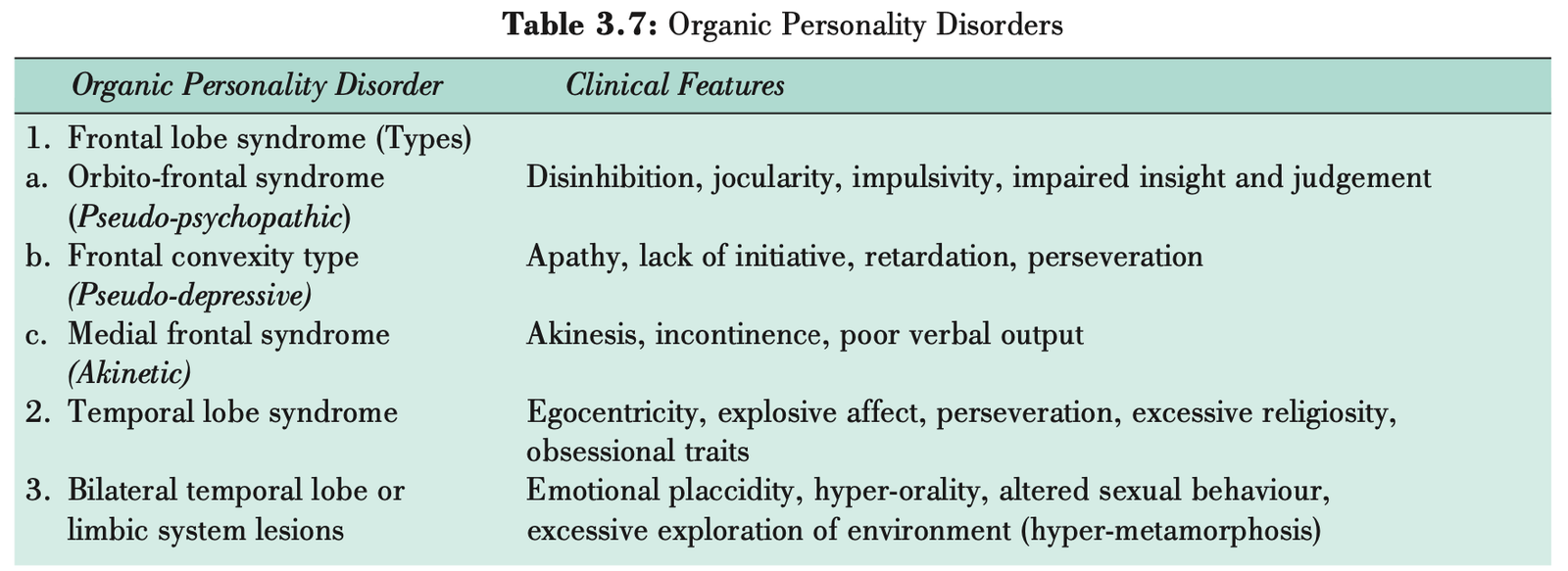
Organic Personality Disorder:
- Characterized by significant alteration of premorbid personality due to an underlying organic cause.
- Diagnosis Criteria (ICD-10):
- Requires an established history or evidence of brain disease, damage, or dysfunction.
- Presence of two or more specific features described.
- Aetiology:
Temporal lobe epilepsy:
- Complex partial seizures associated with temporal lobe epilepsy can lead to temporal lobe (personality) syndrome, as outlined in Table 3.7.
Concussion:
- Concussion may result in postconcussional syndrome, characterized by various cognitive, emotional, and physical symptoms.
Encephalitis:
- Encephalitis can cause postencephalitis syndrome, which may involve mood disturbances among other neurological and psychological symptoms.
Multiple sclerosis:
- Early stages of multiple sclerosis may present with mood disorders alongside other neurological manifestations.
Cerebral neoplasms:
- Neoplasms in the frontal and parietal lobes can lead to frontal lobe syndromes and parietal lobe dysfunction, respectively, as detailed in Table 3.7.
Cerebrovascular disease:
- Cerebrovascular disease, such as strokes or transient ischemic attacks, can precipitate mood disturbances due to brain tissue damage or altered blood flow.
Psychoactive drugs:
- Although rare, certain psychoactive drugs may contribute to mood disorders as a side effect.
Management:
- Treat the underlying cause if treatable.
- Symptomatic treatment with mood stabilizers or antipsychotics may be necessary for aggression or impulse control.
Miscellaneous Organic Mental Disorders:
- Include organic dissociative disorder, organic emotionally labile disorder, and mild cognitive disorder.
- Specific criteria and management for each disorder should be followed as per ICD-10 guidelines.
